Appendix C – The Development of Primary Healthcare in Hong Kong
PHC is the first point of contact for individuals and families in a continuous healthcare process in the living and working community which entails the provision of accessible, comprehensive, continuing, co-ordinated and person-centred care. A well-established and overarching PHC system routinely manages, maintains and enhance the health of the population at the community level, forms the foundation and portal of the pyramid of healthcare services, and serves as a gatekeeping role to specialised secondary and tertiary healthcare in hospital and institution settings. It is recognised as the most essential component in a well-functioning healthcare system.
PHC development in Hong Kong could be traced back to the document Health for all, the way ahead: Report of the Working Party on Primary Health Care in 1990. The Working Party reviewed the Government's role and objectives in health and PHC. It was aware that the Government sector shared 15% of all out-patient medical consultations. With rising public expectations for quality healthcare and need to promote PHC, the “public assistant for all” approach was no longer appropriate. The Government should not aim to become the sole or main provider in primary medical care. The Government’s role should be emphasised on public health and preventive care through multi-sector co-ordinated collaboration, and ensuring and improving the quality and standard of primary care, as well as providing primary care for those who cannot afford private healthcare. The Report affirms the importance of PHC and provided a list of 102 recommendations toward its development.
In the following 10 years, the establishment of the HA in 1990 and the public consultations in 1993 and 199947 had brought the public’s attention to the restructuring of public healthcare services and healthcare financing, which eventually revealed the importance of PHC reform again in 2000, with the release of the consultation document Lifelong Investment in Health. The recommendations include strengthening preventive care, developing Chinese medicine services, transferring the DH’s GOPCs into the HA for integration of primary and secondary care in public sector, and developing electronic Health Information Infrastructure.
In 2005, the Health and Medical Development Advisory Committee reviewed the service delivery model for the healthcare system, and issued a discussion paper Building a Healthy Tomorrow. The recommendations include promoting the concept of family doctor, the target services of public healthcare, purchasing primary care services from the private sector, and facilitating the collaboration among healthcare professionals for co-ordinated care.
Building on the recommendations, the Government put forward a comprehensive proposal in Your health Your life Consultation Document on Healthcare Reform and published the Report on First Stage Consultation in 2008. The recommendations include establishing a family doctor register, developing basic models for primary care services, promoting PPP, subsidising target groups for preventive care, and purchasing primary care services from private sector. The principles of good primary care received positive feedback from the public and healthcare stakeholders. Some respondents expressed support to the establishment of a PHC authority for the planning, co-ordination and governance of PHC services. The Government reconvened the Working Group on Primary Care (WGPC) and three Task Forces under the WGPC to advise on strategic directions for primary care development in 2008.
Based on the strategies and recommendations proposed by WGPC and its Task Forces, the Government published the Our partner for better health – Primary Care Development in Hong Kong: Strategy Document in 2010. The recommendations include setting up a Primary Care Office (PCO), developing Reference Frameworks and Primary Care Directory, and piloting Community Health Centres and networks to devise service models with comprehensive and co-ordinated PHC services through cross-sectoral collaboration in the community.
Following the announcement in the 2017 Policy Address, the Steering Committee on Primary Healthcare Development was set up in November 2017 to develop the blueprint for the sustainable development of PHC services for Hong Kong.
In the 2017 and 2018 Policy Addresses, it was announced that the Government is committed to enhancing district-based PHC services in order to effectively change the current focus of healthcare services on treatment to alleviate the pressure on public hospitals by setting up DHCs in 18 districts progressively. Against this backdrop, the PHO was established on 1 March 2019 directly under the HHB to oversee and steer the development of PHC services at the bureau level. PHO focuses on the development of DHCs as a new service model and spearheads the overall review and future development of PHC services. With the setting up of PHO, PCO was formally integrated into PHO in October 2019 to allow better use of healthcare resources and to streamline the roles and responsibilities of the two offices.
The development of PHC in Hong Kong is briefly illustrated in Figure C.1. The recommendations in the policy and consultation documents for PHC development since the Report in 1990 is set out in Figure C.2.
Figure C.1
PHC Development in Hong Kong
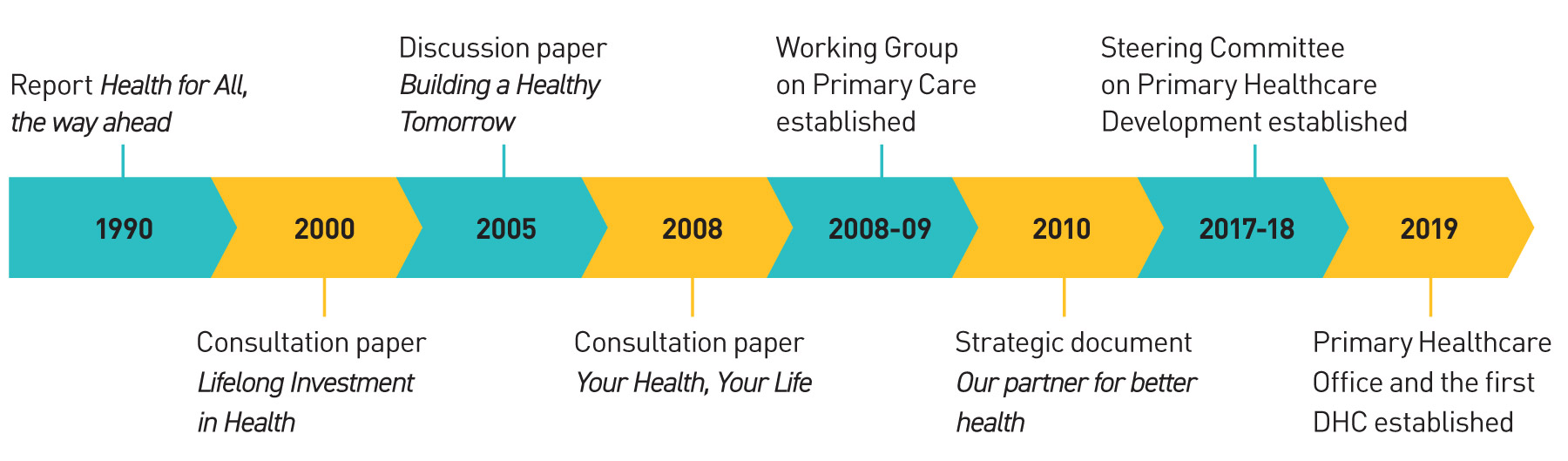
Table C.2:
The recommendations in the policy and consultation documents for the development of PHC
Recommendations
| Policy areas | Health for all, the way ahead: Report of the Working Party on Primary Health Care (1990) |
Lifelong Investment in Health consultation document (2000) |
Building a Healthy Tomorrow discussion paper (2005) |
Your Health, Your Life - Healthcare Reform Consultation Document and Report on First Stage Consultation (2008) |
Our partner for better health – Primary Care Development in Hong Kong: Strategy Document (2010) |
Policy Addresses in 2017 and 2018 |
|---|---|---|---|---|---|---|
| Governance and quality assurance |
|
|
|
|
|
|
| Development of preventive and promotive PHC services |
|
|
|
|
|
|
| Service co-ordination and collaboration |
|
|
|
|
|
|
| Development of district health system |
|
|
|
|
|
|
| Financing of PHC services |
|
|
|
|
||
| Manpower supply and training for PHC |
|
|
|
|
|
|
| Data connectivity and health surveillance |
|
|
|
|
|
|
47 The Government invited public comments on the consultation document Towards Better Health - A Consultation Document about compulsory comprehensive insurance in 1993. The debate continued with the release of Harvard Report to recommend health security plan and saving accounts for long-term care and the consultation document Improving Hong Kong’s HealthCare System: Why and For Whom in 1999.
48 (1) Preventive care, including immunization, maternal and child care, family planning, student health and other services for the control of diseases should be free of charge; (2) Primary care, including screening, for those who cannot afford to pay (e.g. recipients of public assistance) should be free of charge; (3) Screening for elderly and at-risk groups aged 45 to 64 in GOPC and Well-woman Clinics should be at reduced charges; (4) Primary care for young children aged 0 to 15, full-time students up to the age of 18, elderly aged 65 and above, and recipients of disability allowance, should be half fee; (5) Community rehabilitation services, community nursing service and domiciliary occupational therapy service should be of high subsidisation level; and (6) Non-target group should not be charged above the cost.