Ageing Population and Increase in Chronic Disease Prevalence
Like many other places, Hong Kong is facing major challenges brought on by a rapidly ageing population and an increase in the prevalence of chronic diseases. Hong Kong has one of the most rapidly ageing of population in the world and the speed of ageing will peak in the upcoming decade. The average annual increase rate of the population aged 65 and over will be 4.0% from 2021 to 2030 [2, 3]. The population aged 65 and over will increase from 1.5 million (20% of the total population) in 2021 to 2.52 million (31% of the total population) in 2039 [3]. The proportion of old-old (aged 80 and over) will also rapidly increase from 0.4 million (5%) in 2021 to 0.93 million (11.5%) in 2039 [3]. Meanwhile, the elderly dependency ratio2 will double in 2039 [3]. With more than one in three elderlies either living alone or with only an elderly partner [4], social support and carer support for them in the coming decades will be a critical concern.
2 The number of elderly aged 65 and over per 1 000 persons aged 15 to 6 643.
Figure 1.1:
Projection of population aged 65 and over, 2019-2069
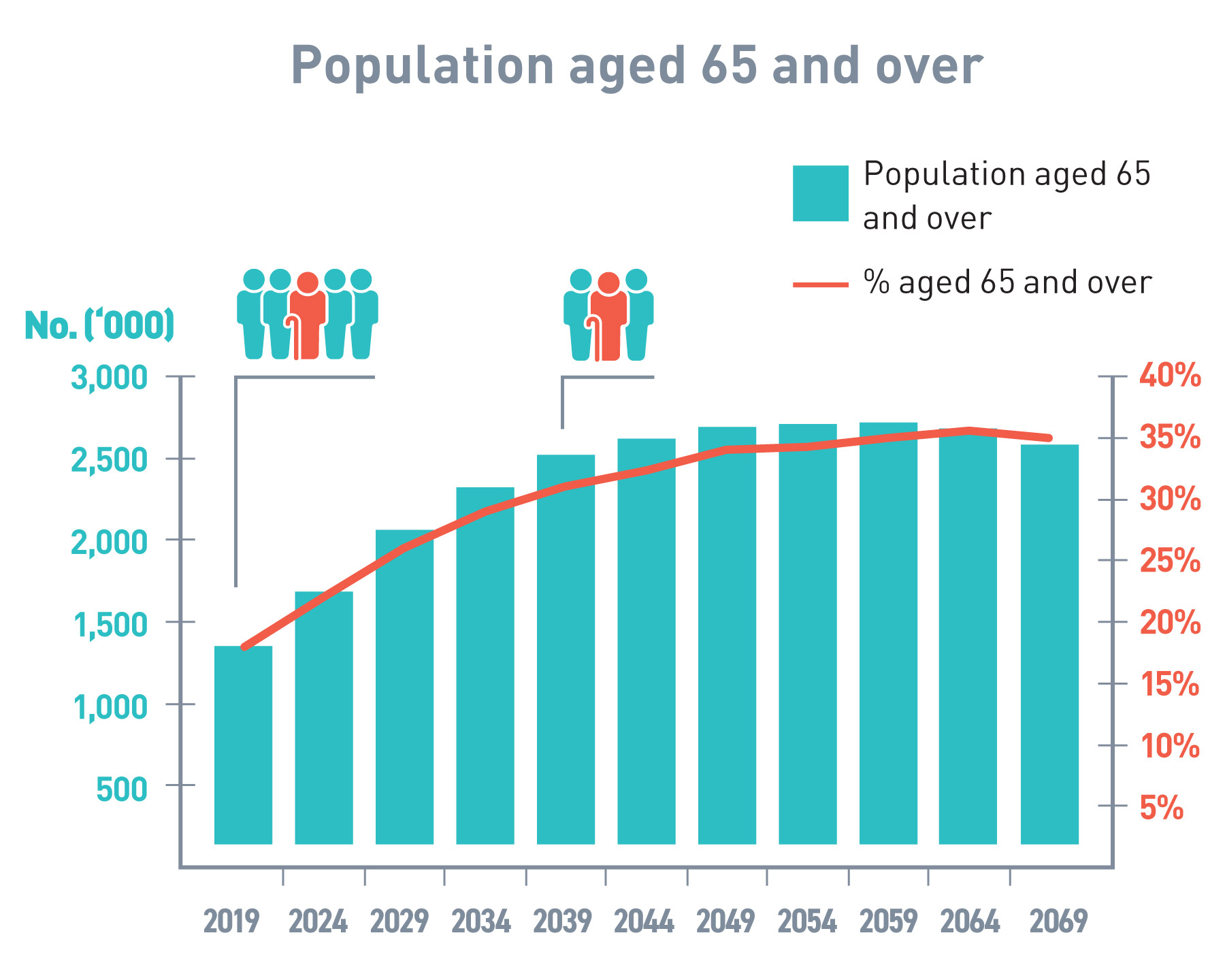
Source: Census and Statistics Department (C&SD) [3]
Ageing is also associated with increasing health and social care needs and higher prevalence of chronic diseases. The percentage of people who had chronic health conditions was 31% (around 2.2 million) in 2020/21, among which 47% were aged 65 and over [5]. The number of Hospital Authority (HA) patients with chronic diseases3 is projected to reach 3 million in the coming decade by 2039. More alarmingly, a substantial number of patients with chronic diseases – believed to be as many as a double of the diagnosed number–remain undiagnosed and unmanaged [6].
About 55% of deaths in Hong Kong are attributable to chronic diseases in 2020 such as HT, heart disease, DM and chronic respiratory problems. Among the most common types of chronic diseases, HT and DM are the highest in prevalence especially among the aged [6].
3 With one of the 25 common chronic diseases: HT, DM, hyperlipidemia, coronary heart disease, stroke, chronic obstructive pulmonary disease, chronic heart failure, chronic kidney disease (stage 3a To 5), glaucoma, osteoporosis (approximated by hip fracture), hepatitis B, depression, dementia, parkinsonism and cancers of the colorectal region, breast, lung, liver, prostat e, cervix, corpus, ovary, nasopharynx, stomach and non non-hodgkin lymphoma.
Figure 1.2:
Ageing population and chronic disease prevalence, 2002-2021
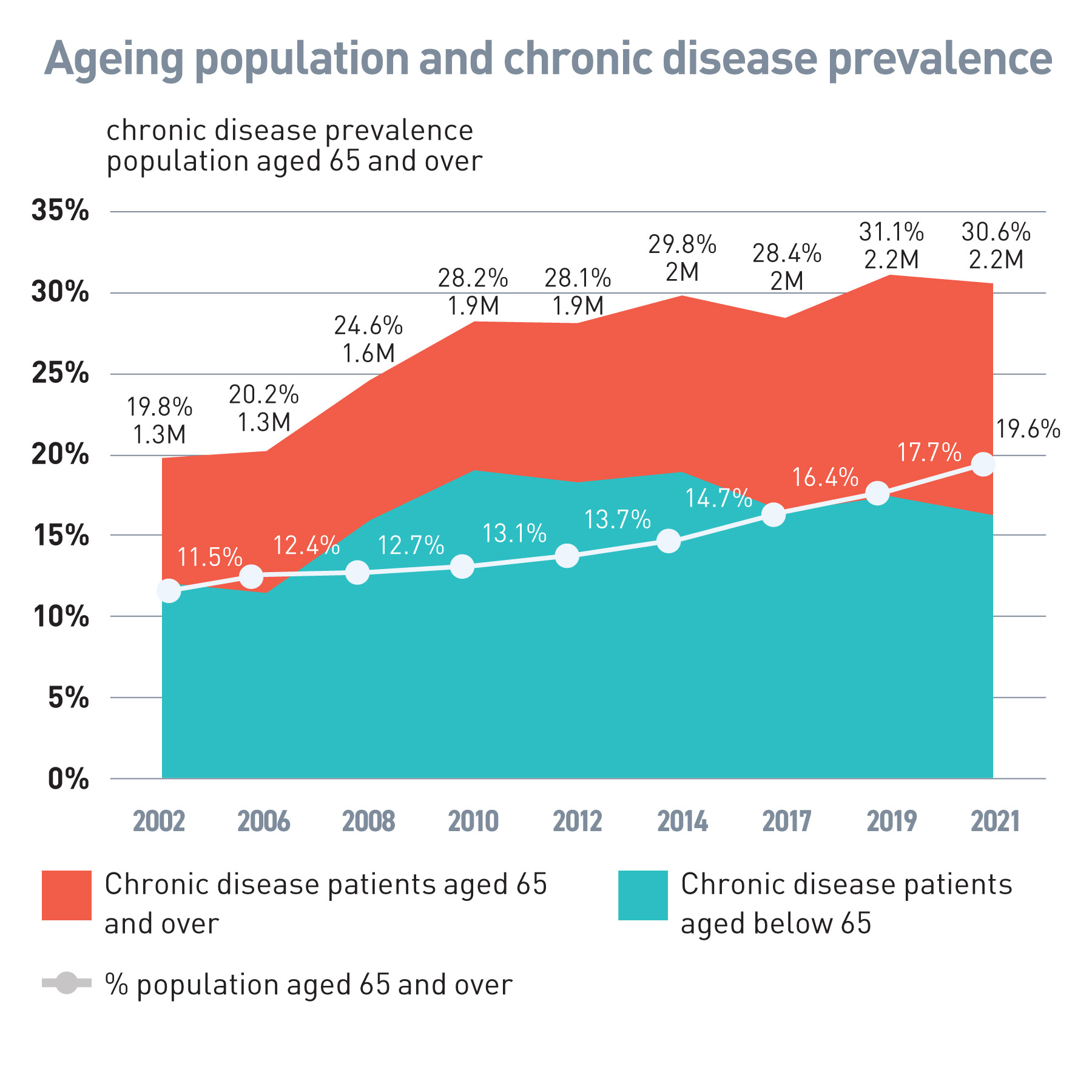
Source: C&SD and Thematic Household Survey Reports No. 12, 30, 41, 45, 50, 58, 63, 68 and 74[2, 5]
Chronic diseases are a major public health concerns because of their impact on quality of life and productivity of the economy due to gradually deteriorating health conditions of the poorly managed patients, as well as their heavy burden to the public healthcare system in terms of high service utilisation and financial cost, especially when the associated complications are not timely intervened. For instance –
- Service utilisation: In 2019/20, for non-cancer chronic disease patients under treatment in the HA’s out-patient settings, namely the General Out-patient Clinics (GOPCs), Family Medicine Specialist Clinics (FMSCs) and Specialist Out-patient Clinics (SOPCs), 82% of them had HT/DM. Among this group, about one-third had cardiovascular disease (CVD) or chronic kidney disease (CKD)4, complications that are associated with HT/DM;
- Service cost: The annual average HA service cost in 2019/20 for patients with HT/DM and related CVD/CKD complications was almost two times higher than patients with HT/DM but without complications; and
- Financial burden: Among patients in the top decile of annual average HA service cost in 2019/20, 60% of them had HT/DM.
4 Including Coronary Heart Disease, Stroke, Chronic Heart Failure and stage 3a to stage 5 Chronic Kidney Disease
Figure 1.3:
Proportion of population with HT and/or DM, 2010-2021
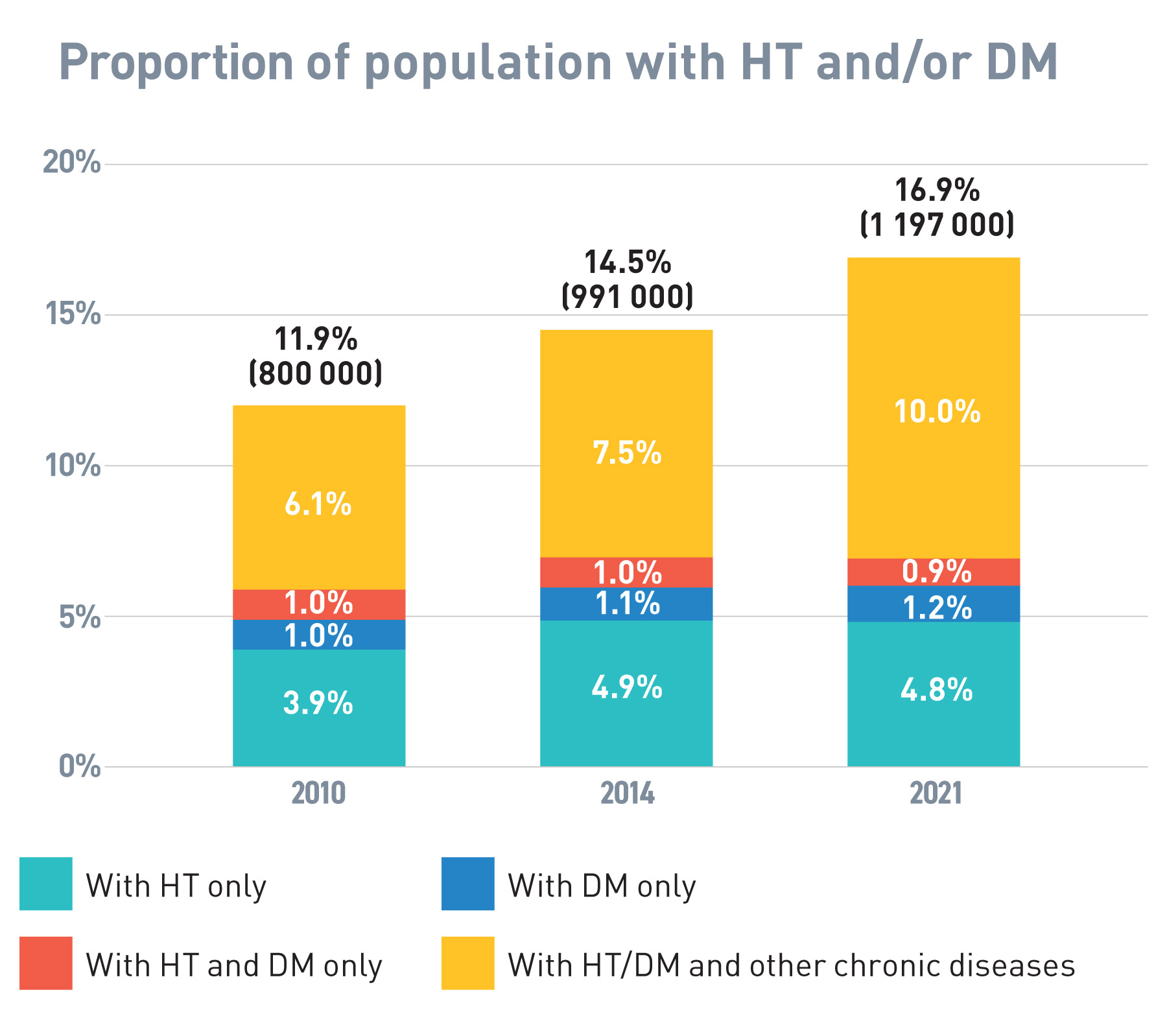
Source: Thematic Household Survey Reports No. 45, 58 and 74 [5]
Health System Sustainability
Hong Kong’s healthcare system is underpinned by a robust public sector and a burgeoning private sector which operate along a dual-track. Public healthcare service is the cornerstone of Hong Kong’s healthcare system, acting as a safety net for the entire community, while the private healthcare sector provides personalised choices and more convenient services to those who are willing and may afford to pay for private healthcare services.
The public sector dominates secondary and tertiary care, accounting for about 63% of the health expenditure of these two tiers combined. It is financed by the Government and its healthcare services are mainly delivered through the Department of Health (DH) and Hospital Authority (HA) [7]. Public healthcare services are heavily subsidised and hence are highly affordable. Details of the healthcare system in Hong Kong is illustrated in Appendix A.
Figure 1.4
Utilisation of GOPC, FMSC and SOPC
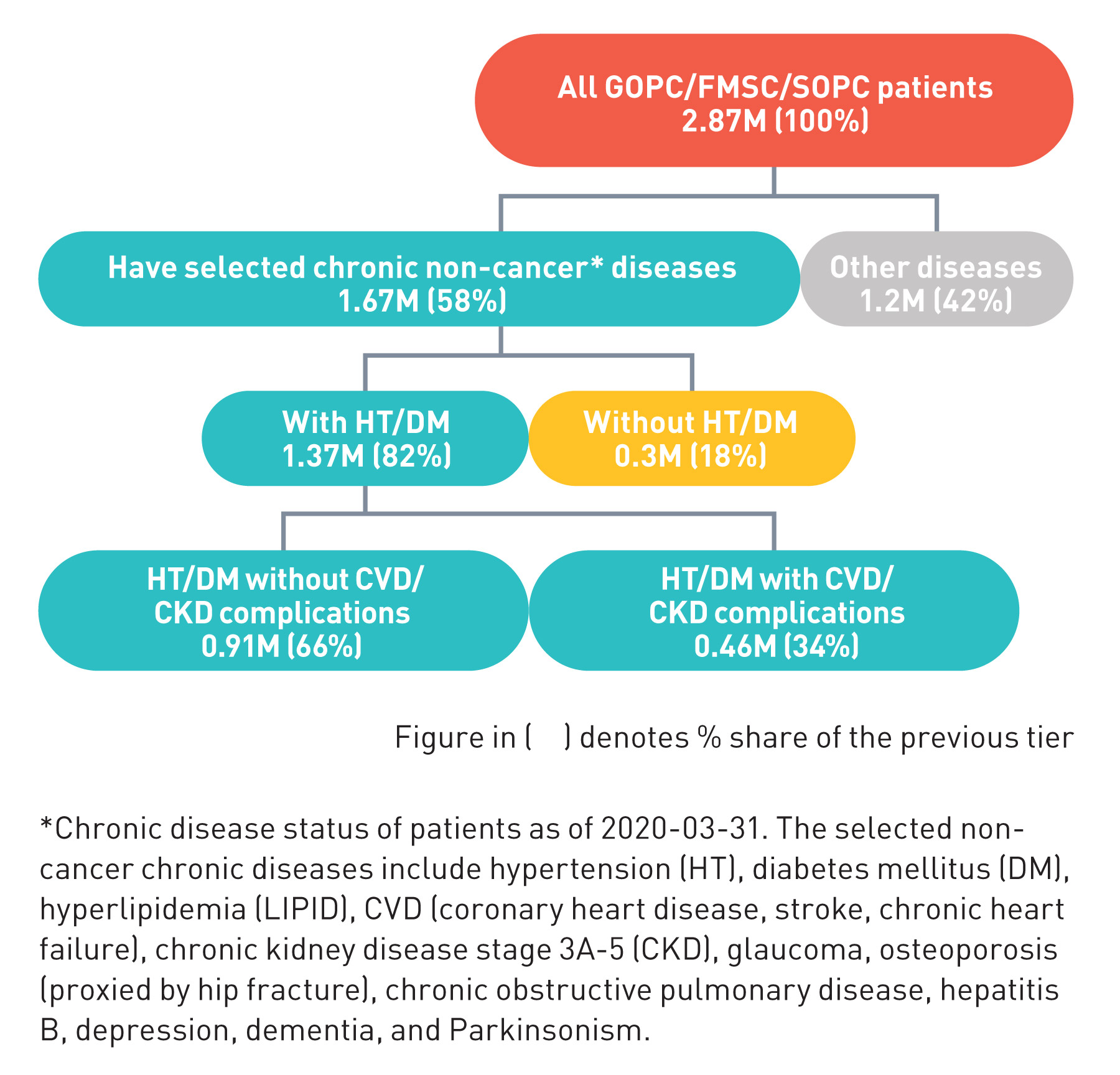
Source: HA data 2019/20
Hong Kong has one of the lowest healthcare expenditure as a percentage of GDP amongst advance economies with comparably demographic profile. In 2019, public health expenditure as a percentage of tax revenue in Hong Kong was among the highest in the world at about 27.1%, while tax revenue as a percentage of GDP was among the lowest at about 12.6% [7, 8]. This is a strong evidence that the healthcare system in HK, despite the increasing expenditure in tandem with the rapidly ageing population, remains a highly cost-effective and efficient one, insofar as it can still deliver healthcare services to meet the needs of the population and maintain HK as having one of the longest life expectancy and lowest infant mortality around the world. However, it is simply unsustainable to keep increasing public health expenditure to fund the public hospital system to cope with the ever-increasing healthcare demand, unless systemic reform to the healthcare system is introduced.
Figure 1.5:
Average HA service cost per patient
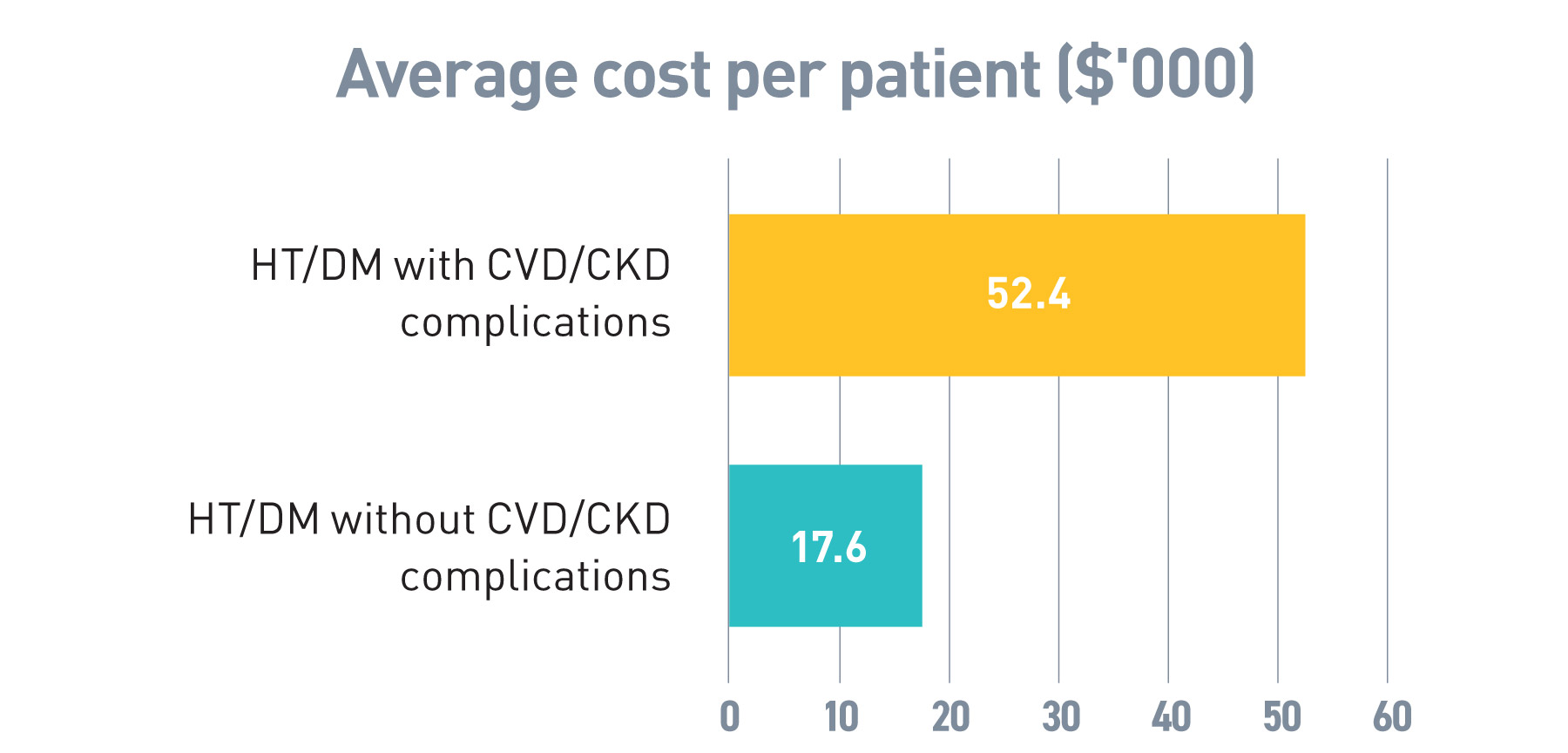
Source: HA data 2019/20
There is no set global standard for the percentage of health expenditure that a health system should be spending on PHC. That said, across the 88 countries analysed in the 2019 WHO “Global Spending on Health: A World in Transition” report, PHC spending ranged from 33% to 88% of health spending, with a global 54% average across the 88 countries.
Currently, treatment-oriented secondary and tertiary healthcare especially public hospital services accounted for the majority of healthcare services and spending in Hong Kong. According to the 2019/20 DHA, the total health expenditure in Hong Kong is roughly split by 30:70 between PHC ($52.9 billion) and secondary/tertiary healthcare ($127.3 billion) which is much lower than the average expenditure of 54% across 88 countries as aforementioned. Owing to heavily subsidised public hospital services at over 97% of costs, public healthcare expenditure is even more concentrated with around 83% ($79.9 billion) of public health expenditure spent on secondary and tertiary healthcare whereas only 17% was spent on PHC ($16.0 billion) [7].
Figure 1.6:
Tax revenue to GDP and public health expenditure to tax revenue in selected economies with similar GDP per capita, 2019/20
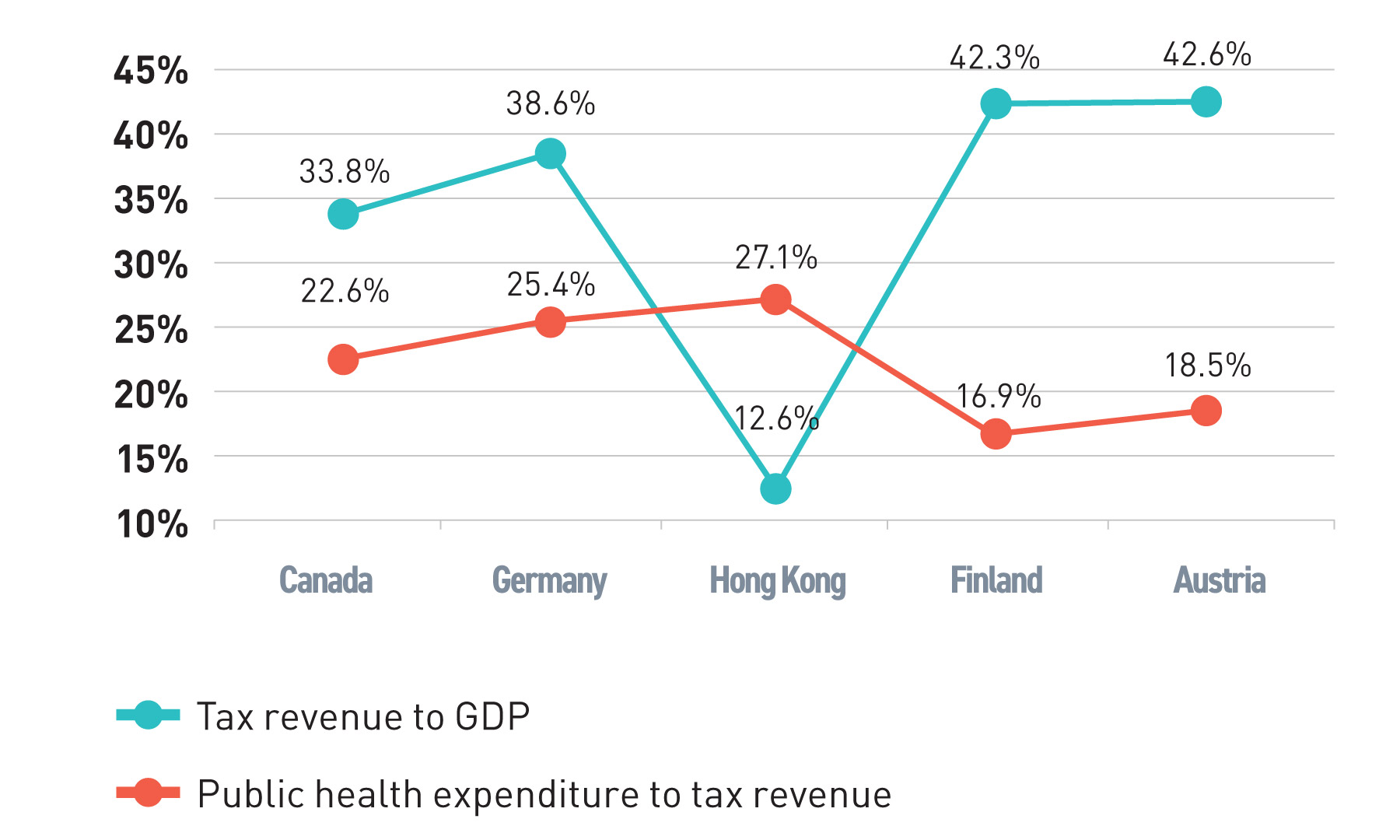
Source: OCED, Domestic Health Accounts (DHA) [7, 8]
Treatment-oriented healthcare induces higher healthcare costs and accelerates the increase of health expenditure. Over the past three decades, both public health expenditure and private health expenditure have been increasing in parallel. More worryingly, health expenditure growth has been exceeding economic growth. From 2010/11 to 2019/20, our average annual growth rate of public health expenditure was 5.6% faster than that of GDP at 2.0% in real terms [7]. According to the projection based on a research done in 2008 commissioned by the then Food and Health Bureau [1], it was estimated that total/public healthcare expenditure will increase from 5.3%/2.9% of GDP in 2004 to 7.1%/4.1% of GDP in 2020 if nothing was done to reform the healthcare system. Actual total/public healthcare expenditure (excluding COVID-19 expenditure) was estimated to be about 6.7%/3.6% of GDP in 2019/20 according the Domestic Health Accounts, illustrating that various reforms over the years might have helped to curb the expenditure increase. Having said that, the accelerating ageing of the population in the coming decade will on the one hand further limit GDP growth and the budget for public health expenditure, and on the other increase the demand for public health spending.
Figure 1.7:
Composition of current health expenditure
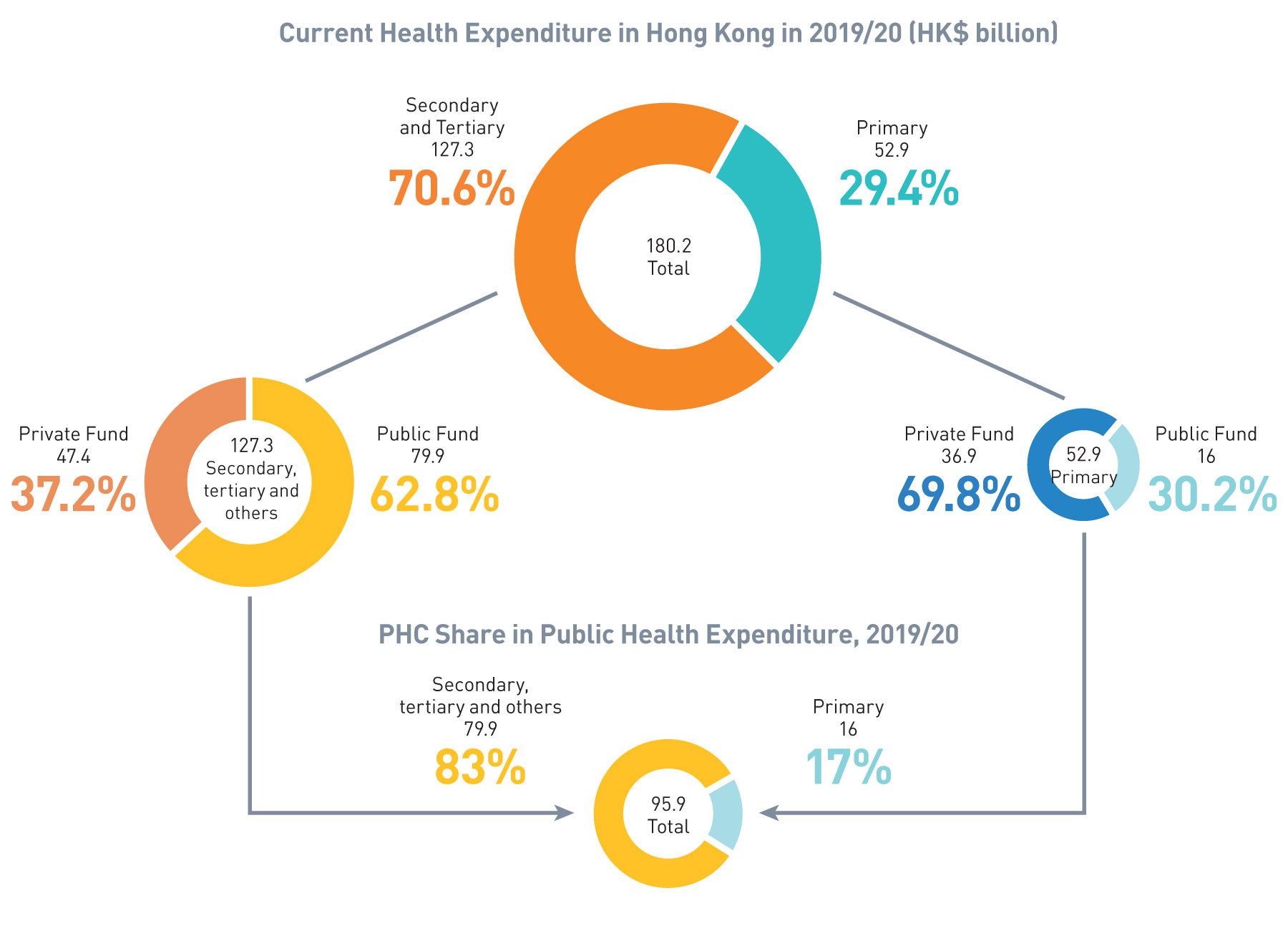
Source: DHA[7]
Hong Kong’s public healthcare system has posed a threat to sustainability. The growth of public health expenditure and current health expenditure has been largely exceeding the growth of GDP over the previous decade [7]. The situation will be further aggravated with the rapid ageing of the population and the rising chronic disease prevalence in the upcoming decade. Our healthcare system will not be sustainable unless a systemic change is being introduced. A more strategic allocation of public health expenditure is critical.
Figure 1.8:
The growth of public health expenditure and GDP in real terms
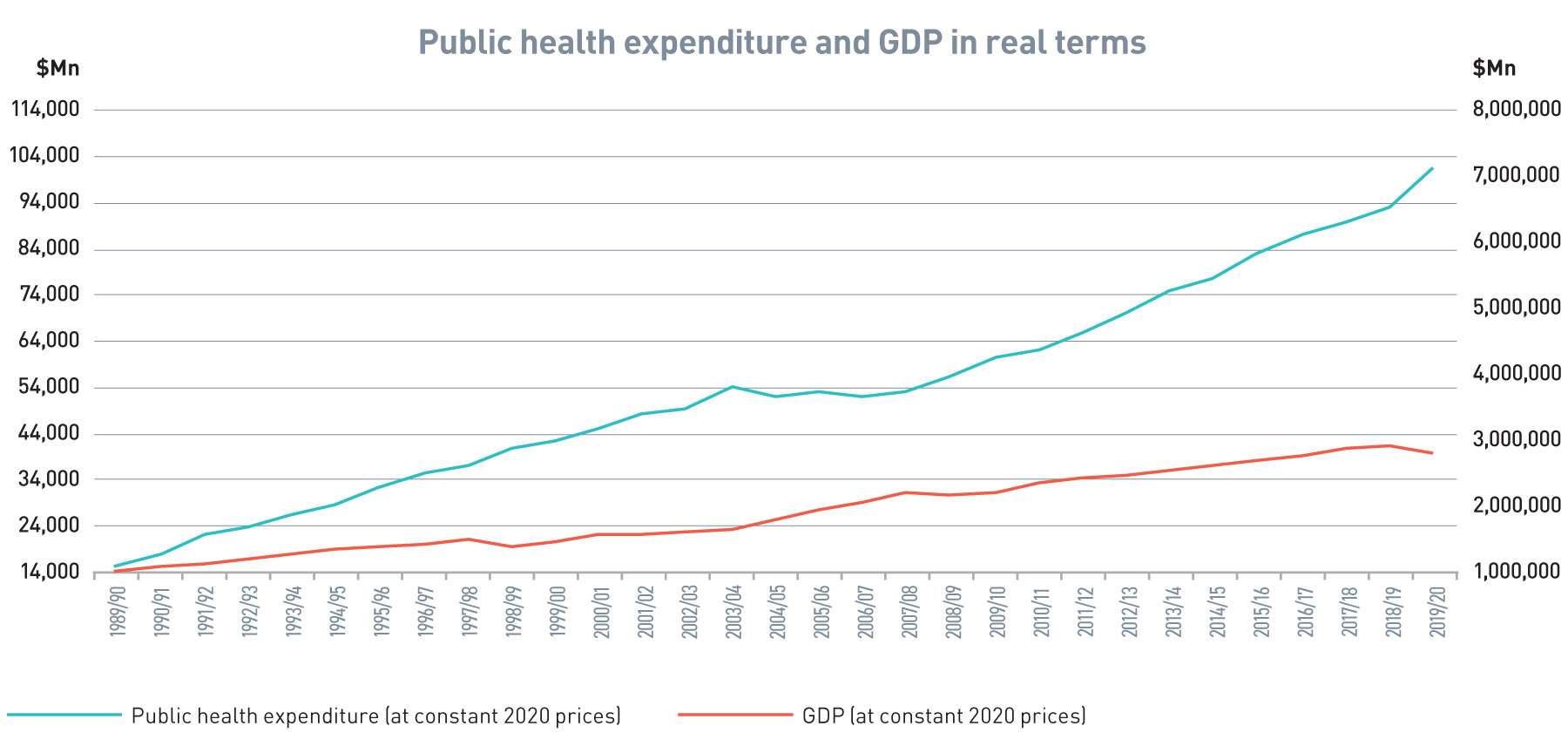
Source: DHA
Public Healthcare System at Risk
Faced with both an ageing population and an increase in chronic disease prevalence, the health and social care needs of our community will increase significantly in the coming years. To achieve better population health and quality of life, we need to shift the centre of gravity of our healthcare system from treatment-oriented institution-centric secondary/tertiary healthcare to prevention-oriented family-centric PHC. Through well-managed healthcare at community level, we envisage that chronic disease patients’ medical and health needs will be properly taken care of at the community level. In turn, alongside longevity, their physical well-being and quality of lives will be enhanced, their morbidity will be compressed and their needs for hospital care will be reduced and deferred. The overall health status of the population shall thereby be improved.
Figure 1.9:
A&E first attendance in 2021/22
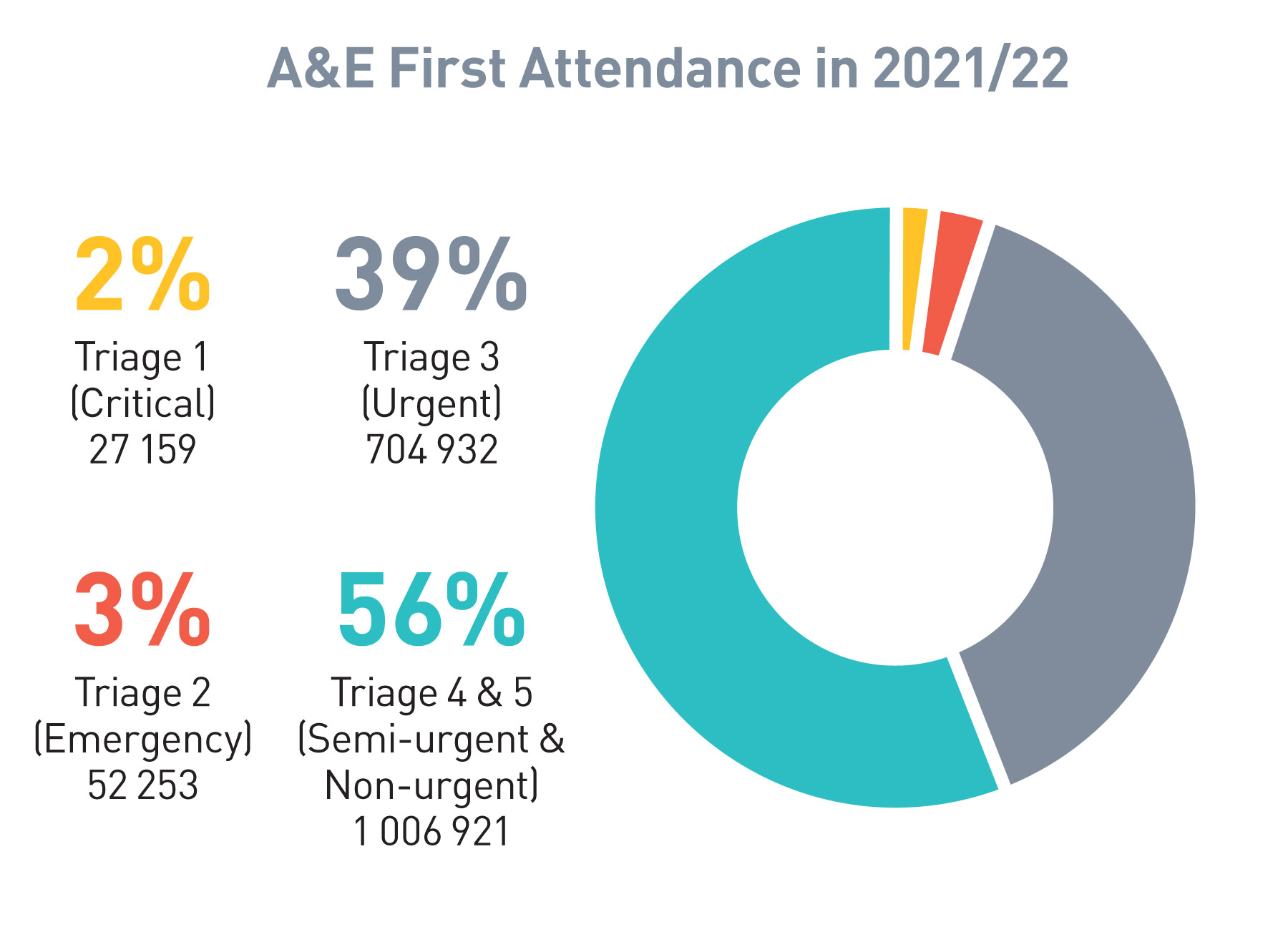
Source: HA data 2021/22[10]
Potentials of the Private Primary Healthcare Sector and public-private partnership
Complementing the public healthcare system, the private sector is the chief provider of PHC, accounting for about 68% of the out-patient doctor consultation market in Hong Kong [5, 7]. Primary care in the private sector comprises a wide selection of private service providers. They include general and specialist clinics as well as Chinese Medicine (CM) clinics, dental clinics, community pharmacies, diagnostic centres, medical laboratories, optical shops, etc. Choice is a cornerstone in private services. Patients, at their own expenses (with some under private insurance coverage), are free to choose their preferred doctors and other service providers according to their own needs and preferences. Other advantages over the public healthcare system include shorter waiting time, better environment, more convenient service locations, and more personal and tailored services where necessary.
The private sector, funded mainly by private funds, is the major provider of PHC services, accounting for about 75% of PHC expenditure and about 68% of out-patient doctor consultations. In 2019/20, about 77% of private health expenditure on PHC was paid out-of-pocket [5, 7].
Figure 1.10:
Out-patient attendance
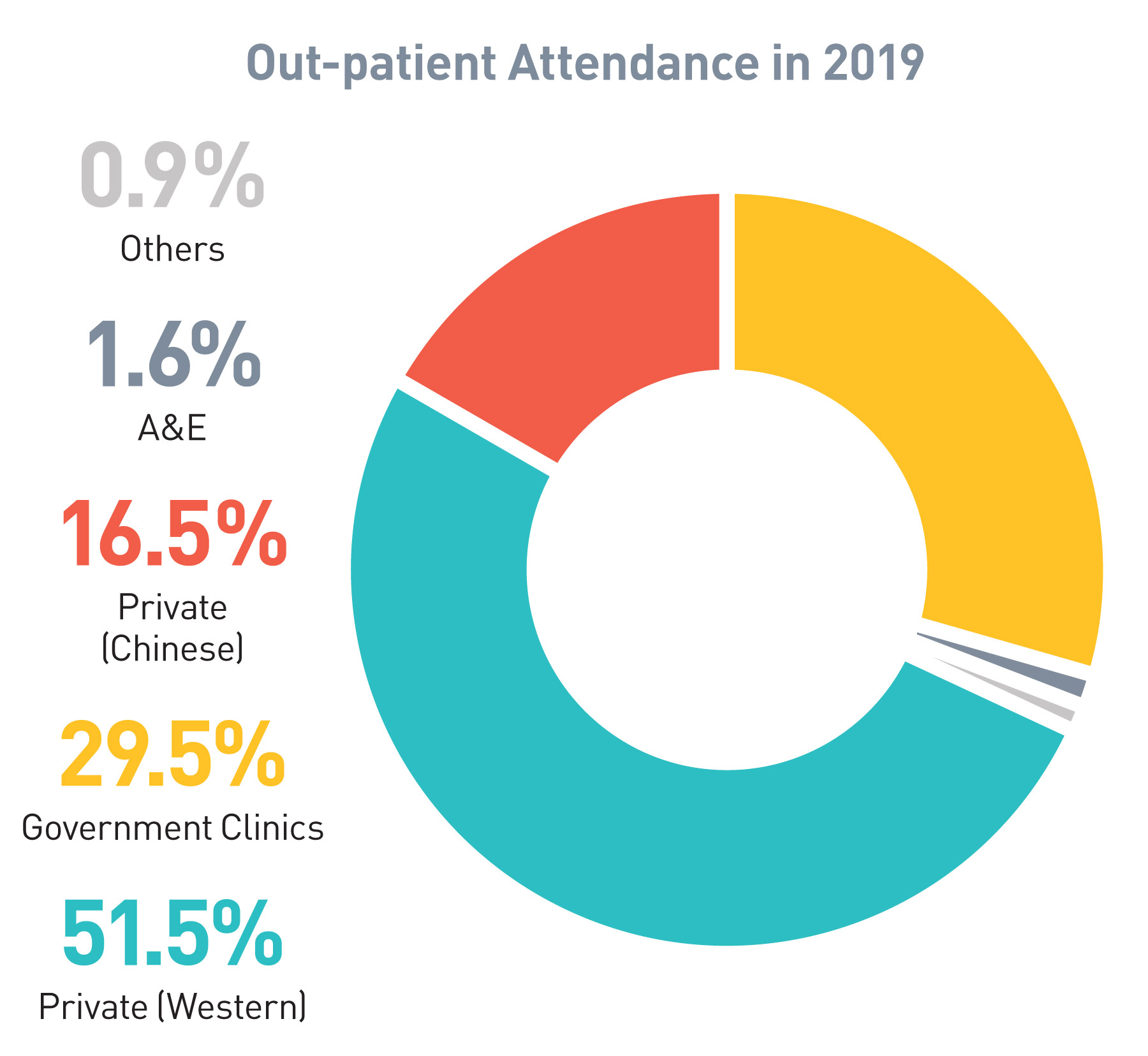
Source: Thematic Household Survery Report No. 68[5]